Cartilage Defect Treatment Using High-Density Autologous Chondrocyte Implantation: Two-Year Follow-up
Publicado en: Cartilage
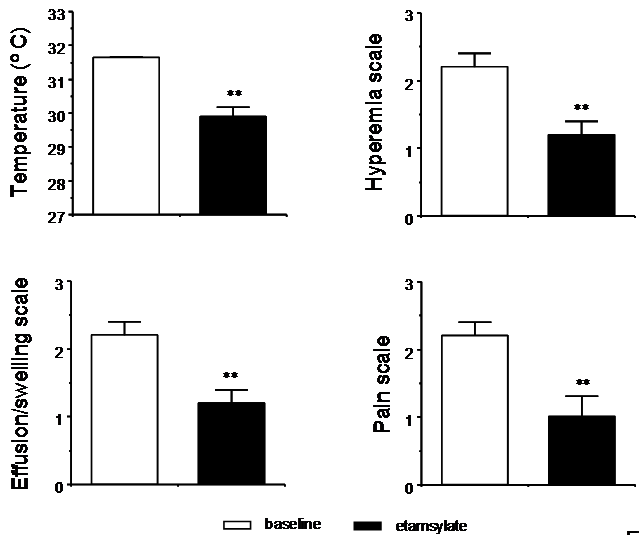
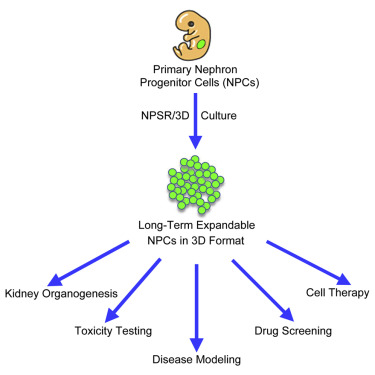
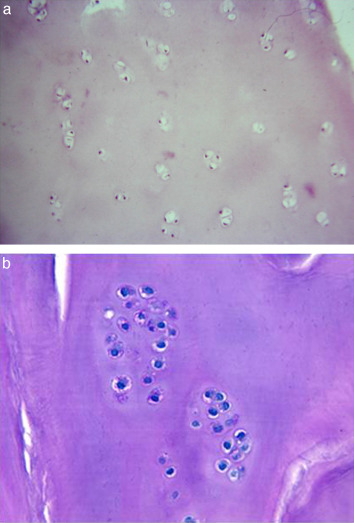
Objective. The aim of this work was to study the short- and mid-term effectiveness and safety of high-density autologous chondrocyte implantation (HD-ACI) in the first 50 patients with knee cartilage damage treated in our unit. Design. Fifty consecutive patients with cartilage lesions (Outerbridge grade III-IV) in the knee treated with HD-ACI were included in this study. Chondrocytes were isolated from a nonbearing cartilage area biopsy and were cultured until 40 to 50 million cells were obtained. Five million chondrocytes per cm2 of a porcine collagen type I/III membrane were implanted covering the defect. Procedure effectiveness was assessed by evaluating pain, swelling, and range of mobility (flexion and extension) at 6-, 12-, and 24-month follow-up. The International Knee Documentation Committee (IKDC) subjective evaluation form was used to evaluate symptoms and functions of the knee. Results. The percentage of patients with pain and swelling decreased progressively in the following visits, with differences being statistically significant (P < 0.001 and P = 0.040, respectively). IKDC scores improved progressively throughout the 24-month follow-up (P < 0.001). Thus, the mean IKDC score improvement was 26.3 points (95% confidence interval [CI] = 18.2-34.4 points) at 12 months and 31.0 points (95% CI = 22.9-39 points) at 24 months. No significant differences were found when performing extension (P = 0.112). Flexion significantly improved by 25.1° at 24-month follow-up (P = 0.013). Conclusions. HD-ACI is a safe and effective technique for the treatment of cartilage defects, improving clinical and subjective perception of knee functionality. These preliminary results encourage future studies comparing this technique with traditional ACI.
Referencia:
J.M. López-Alcorocho, L. Aboli, I. Guillén-Vicente, E. Rodriguez Iñigo, M. Guillén-Vicente, T. F. Fdez.-Jaén, S. Arauz, S. Abelow and P. Guillén-García. “Cartilage Defect Treatment Using High-Density Autologous Chondrocyte Implantation: Two-Year Follow-up” Cartilage 1-7 DOI:10.1177/1947603517693045
Link: http://journals.sagepub.com/doi/abs/10.1177/1947603517693045